Overview of Acute Coronary Syndrome (ACS)
10/01/2021
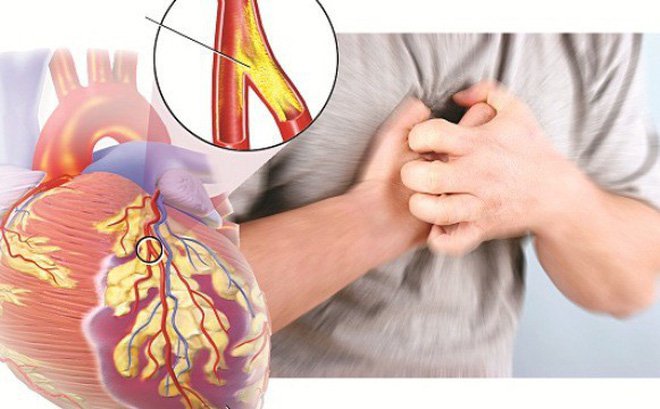
Acute coronary syndromes due to coronary artery occlusion. Outcomes depend on the extent and location of the obstruction and range from unstable angina to non-ST-elevation myocardial infarction (NSTEMI), acute ST-elevation myocardial infarction (STEMI), and death. sudden cardiac arrest. Symptoms are similar in each of these syndromes (except sudden death) and include chest discomfort with or without dyspnea, nausea, and sweating.
Diagnosis is by ECG and the presence or absence of serological markers of cardiac enzymes. Treatment is antiplatelet agents, anticoagulants, nitrates, beta-blockers and, for STEMI, urgent coronary reperfusion through fibrinolytics, percutaneous interventions, or occasionally, surgery coronary artery bypass.
- Classify
Acute coronary syndromes include:
- Unstable angina
- Non-ST-elevation myocardial infarction (NSTEMI)
- ST elevation myocardial infarction (STEMI)
These syndromes are associated with acute coronary ischemia and are differentiated on the basis of symptoms, ECG findings, and elevations of cardiac enzymes. It is helpful to differentiate the syndromes because of the different prognosis and treatment.
Unstable angina (coronary insufficiency, history of acute infarction, intermediate syndrome) is defined as one or more of the following in patients with cardiac biomarkers who do not meet the following criteria: Criteria for myocardial infarction:
- Persistent angina at rest (usually > 20 minutes)
- New-onset angina of at least grade 3 severity in the Canadian Heart Association (CCS) classification (see Table: Canadian Cardiovascular Society Classification of Angina)
- Increased angina, i.e., previously diagnosed angina that has become evident more often, worsens, persists longer, or is below the threshold (eg, ≥1 CCS grade elevation or at least CCS grade elevation 3)

ECG changes such as ST-segment depression, ST-segment elevation, or T-wave inversion can occur during unstable angina but they are transient. Cardiac markers, CK are not elevated but cardiac troponin, especially as measured by highly sensitive troponin assays (hs-cTn), may be slightly elevated. Unstable angina is clinically unstable and is often a symptom of myocardial infarction or arrhythmia or, less commonly, sudden death.
Non-ST-segment elevation myocardial infarction (NSTEMI, subendocardial MI) is myocardial necrosis (as evidenced by cardiac markers in blood, troponin I or troponin T and CK elevations) without acute ST-segment elevation . ECG changes such as ST segment depression, T-wave inversion, or both may be present.
ST-elevation myocardial infarction (STEMI, transmural MI) is myocardial necrosis with ECG changes showing ST elevation without rapid reversal by nitroglycerin or the development of new left bundle branch block. Cardiac markers, troponin I or troponin T, and CK are increased.
Both types of MI may or may not produce Q waves on the ECG (Q wave MI, non-Q wave MI).
2. Cause
The most common causes of acute coronary syndrome are: A severe thrombosis in the coronary arteries due to atherosclerosis. Plaque may be unstable or inflamed, cause rupture or division, expose thrombotic elements, activate platelets and staphylococci to coagulate and produce thrombosis. Platelet activation involves a structural change in the membrane glycoprotein (GP) receptor IIb/IIIa, which allows cross-linking (and thus association) of platelets. Even minimally occlusive atherosclerotic plaques can rupture and result in thrombosis; In >50% of cases, pre-event stenosis is <40%. Thus, although the severity of stenosis helps predict symptoms, it does not always predict thrombotic events. The resulting thrombus suddenly interferes with blood flow to parts of the heart muscle. Spontaneous hemolysis occurs in about two thirds of patients; Twenty-four hours later, thromboembolic obstruction is found in only about 30%. In most cases, however, the obstruction persists long enough to cause tissue necrosis.

Rarer causes of acute coronary syndromes are:
- Coronary artery occlusion
- Coronary spasm
Coronary embolism can occur in aortic or aortic stenosis, infective endocarditis, or endocarditis. Cocaine use and other causes of coronary artery spasm can sometimes lead to MI. MI can occur in normal or atherosclerotic coronary arteries.
3. Pathophysiology
Initial outcomes vary with the size, location, and duration of the obstruction and range from transient ischemia to infarction. Measurement of newer, more sensitive markers shows that some cell necrosis can occur even in mild form; therefore, ischemic events occur continuously, and classification into subtypes, although useful, is somewhat arbitrary. The sequelae of the acute event depend mainly on the volume and type of heart tissue infarcted.
Cardiac dysfunction: The ischemic (but not infarcted) tissues have decreased contractility and dilation, resulting in reduced or no movement of the vascular myocardium, the lungs, the dilated or bulging areas of the myocardium. during systole (known as paradoxical movement). The size of the affected myocardium determines the severity from minimal to mild from heart failure to cardiogenic shock; Normally, much of the right myocardium is ischemic causing severe myocardial dysfunction. Some degree of heart failure occurs in about two-thirds of patients hospitalized with acute myocardial infarction. It is called ischemic cardiomyopathy if ventricular output and heart failure are persistent. Ischemia involving the papillary muscle will lead to mitral regurgitation. Paradoxical movement of the myocardium wall can cause a thrombus in the heart chambers.

Myocardial Infarction (MI): Myocardial infarction is necrosis of the heart muscle caused by a sudden decrease in coronary blood flow to that part of the heart muscle. Infarct tissue is permanently inactive; however, there is an area of potentially reversible ischemia next to the infarcted tissue. Myocardial infarction affects mainly the left ventricle (LV), but damage can spread to the right ventricle (RV) or atria. Infarction may be transmural or non-transmural. Transmural MIs related to myocardial thickness from the pericardium to the endocardium of the myocardium are characterized by the appearance of necrotic Q waves on ECG. Non-transmural MI or subendocardial MI does not extend through the ventricular wall and causes only ST segment and T-wave abnormalities (ST-T). Because the depth of necrosis of the necrotic myocardium cannot be determined precisely, infarctions are usually classified as STEMI or NSTEMI by the presence or absence of ST-segment elevation or upper Q waves. ECG. Necrosis of a substantial portion of the ventricular septum or parietal muscle can rupture, with dire consequences. A ventricular aneurysm or pseudoaneurysm may develop after an acute MI.
Electrolyte disturbances: Electrical dysfunction can be significant in any type of ACS patient. The ischemic and necrotic cells are incapable of normal electrical activity, leading to various ECG changes (mainly ST-T abnormalities), arrhythmias, and conduction disturbances. The ST-T mutations of anemia include ST-segment depression (usually descending from the J-point), T-inversion, ST-segment elevation (commonly referred to as trauma), and giant peak T waves in the acute phases of MI. Conduction disturbances may reflect damage to the sinus node, atrioventricular (AV) node, or specific conducting tissues. Most changes are transient; some are permanent.
Bài viết liên quan
- How dangerous is prostate cancer?
- Septicemia: Causes, signs and treatment
- Hemophilia: Causes, symptoms, diagnosis and treatment
- 6 things to know about cervical cancer
- Hyperthyroidism and cardiovascular complications
- Some things to know about high blood pressure
- 70% of people with diabetes in Vietnam have not been diagnosed
- Patient satisfaction is top priority: Prime Minister
- Local residents get free medical service



